How Does Cholesterol Affect Digestion?
Posted by Andrea Nakayama
Cholesterol can be confusing. Is it good? Is it bad? Is my cholesterol too high? Is my cholesterol too low? Confusing matters more, what’s the role of cholesterol on digestion?
Whenever I encounter one of these confusing topics, I delve into the science of it, particularly the physiology. Far more than any dietary theory (which can’t and won’t work for every body) understanding the science — the physiology — is a key ingredient for using food as medicine.
How does cholesterol affect digestion and bile acids?
When we consume fats in any form, they are initially broken down in the form of triglycerides. Chemically, triglycerides are a fatty acid molecule attached to a glycerol backbone. In our stomachs, which is part of our upper digestive system, there is typically some mineral breakdown of fats due to the action of an enzyme called gastric lipase. But the majority of digested fat is digested in our small intestine.
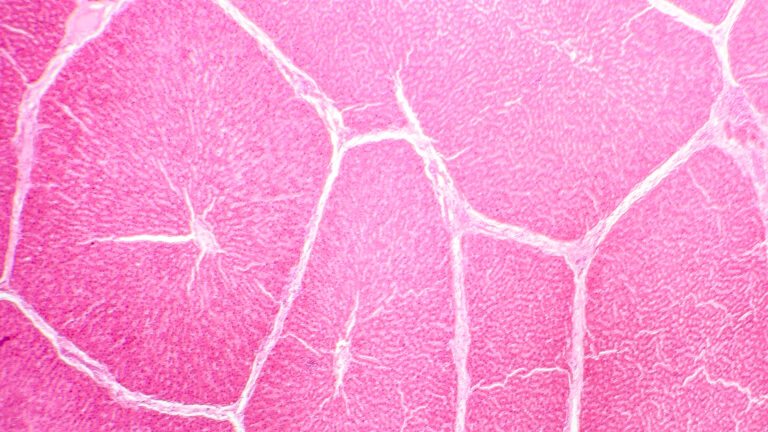
When partially digested food enters the small intestine in the form of chyme, it triggers the release of a hormone called cholecystokinin (CCK). This signals the gallbladder (if we have one!) to release bile. Bile is made up of bile salts, cholesterol, water and other substances.
Cholesterol synthesizes bile acids which are essential for the absorption of fat from the small intestines. The bile acids work like a detergent to break down and emulsify fat into microscopic droplets. Those tiny beads of fat then have enough of an exposed surface area for lipases (your fat digestive enzymes) to come in and do their job of absorbing those fatty acid molecules into your bloodstream to support your energy, cell integrity, and internal insulation.
Cholesterol production in the liver
Most cholesterol is produced in the body by the liver and contrary to dietary myths, does not come from the food you eat, but we’ll bust that myth later. After creating cholesterol, the liver sends out two different agents—LDL (low-density lipoproteins) and HDL (high-density lipoproteins). The LDL travels away from the liver and into the blood and has several functions including:
- protection and repair of cell walls so that they are appropriately permeable (allowing only what is opportune to pass in and out of each and every cell in your body)
- serving as the backbone for many of our sex and stress hormones (think: progesterone, testosterone, estrogen, cortisol)
- production of the bile acids that allows for the vital digestion and absorption of the fats, oils and fat soluble vitamins (like your vitamin D!) from the foods you eat
A key role of HDL is transporting the excess cholesterol from the bloodstream back to the liver for secretion. HDL does the clean-up.
If you made it with me this far, or if you’ve already chewed those facts, then you know cholesterol is vital for good health! Your cells need it. Your hormones need it.
Your digestive tract needs it. Since cholesterol is mostly produced in the liver, the vitality of the liver is critical for maintaining healthy cholesterol levels. When your liver is in good form, it produces more HDL to help with the clean-up of the cholesterol circulating in the blood. That’s why higher HDL is considered good.
The impact of dietary cholesterol
It’s important to remember that cholesterol is produced naturally in the body and plays a critical role in various physiological processes, as previously noted. So where does dietary cholesterol enter the picture?
The myth surrounding dietary cholesterol suggests that when we eat foods that are cholesterol rich, such as egg yolks, shellfish or organ meats, that they’ll translate into high blood cholesterol levels. This is an oversimplification of how the body functions.
The extent to which dietary cholesterol will impact blood cholesterol (measured in your annual lipid panel) varies widely among individuals. For some, there will be no significant impact at all. Others might experience a mild correlation between their dietary cholesterol intake and their serum cholesterol levels.
In fact there are other dietary and lifestyle factors that have a far greater impact on their blood cholesterol, including intake of chemically altered fats, physical activity and unique genetic factors. Even the American Heart Association and the Dietary Guidelines for Americans have now recognized that the causation between dietary cholesterol and blood cholesterol is broadly untrue! And this is why we have to bust the myth that whole foods that contain high amounts of dietary cholesterol are universally “good” or “bad”.
What can be done to improve cholesterol digestion and absorption?
Eat more fiber to support your liver health
Chances are you’ve already heard the ‘eat more fiber’ mantra but it’s my #1 action step for supporting liver health (and therefore your dual actions of your digestion and cholesterol) On average, Americans consume about 1/3 the amount of fiber needed. Fiber binds and transports extra bile acids out of the body so it isn’t reabsorbed by the liver.
Excellent fiber rich foods include:
- vegetables (particularly hearty leafy greens, cauliflower and broccoli)
- fruits (most berries and apples have great fiber)
- seeds (ground flax is a winner and chia has lots of fiber as well)
- beans (lentils, black, pinto, garbanzo, lima)
- grains (oats, quinoa, brown rice, if tolerated)
- and cinnamon too!
Today, tomorrow and heck from here on out, focus on filling up with fiber! And remember, we each digest and absorb fiber differently. If you’re working with someone that is new to consuming more fiber, start low and go slow. Track to see what changes they experience with their digestion and elimination.
References:
EXPERIENCE A FREE TRAINING SERIES WITH ANDREA NAKAYAMA TO HELP YOU
Begin practicing functionally today!
MORE TO EXPLORE
You Might Also Like
Maya Simand: Cancer Survivor to Holistic Cancer Coach
Holistic cancer coach Maya Simand shares her inspiring journey to healing. Discover how Functional Nutrition education empowered her to overcome breast cancer and help others find hope through integrative approaches.
Read MoreEstrogen dominance and breast cancer prevention: A Functional Nutrition approach
Estrogen dominance is a key factor in ER+ breast cancer. This Functional Nutrition guide explores how estrogen dominance increases risk and provides practical strategies to balance hormones and support overall health.
Read MoreThe 3 Roots, Many Branches: A Functional Framework for Clinical Success
As practitioners or aspiring nutrition counselors, we’re all familiar with the frustration of watching people struggle with chronic illness, cycling through symptoms and diagnoses without resolution.
Read MorePutting Patients First with Patient-Centered Care
I recently read an account written by a primary care doctor (PCP) describing a patient who had been passed from one specialist to another—each one focusing on ordering tests, prescribing medications, and ultimately sending her off with more questions than answers. No one paused to truly listen to the patient’s story. No one asked about […]
Read More