The Connection Between Sugar and Inflammation
Posted by Andrea Nakayama
Thousands of years ago the Romans described the major components of inflammation:
- calor (heat)
- rubor (redness)
- tumor (swelling)
- and dolor (pain)
All four of these symptoms are caused by increased blood supply to an infected area. Ergo, inflammation. Let’s dive in and explore the risks and rewards of inflammation.
Inflammation’s role in chronic disease and health challenges
Inflammation is a key part of the body’s immune response. Acute inflammation plays a crucial and beneficial role in the body’s protective mechanisms. It helps with pathogen defense, tissue repair and healing, and the activation of important antibodies that have a role in our long term survival.
Recent discoveries also show that chronic inflammation is a root cause in the development and progression of chronic disease and health challenges. Conditions like heart disease, diabetes, Alzheimer’s, autoimmune disorders and cancer can all be linked to chronic inflammation which can often occur without causing any noticeable pain. Additionally, inflammation is responsible for various everyday health issues, including:
- body aches and pains
- congestion
- irregular elimination
- indigestion
- skin outbreaks
- frequent infections
- advanced aging
- arthritis
- weight gain & weight loss resistant
In other words, inflammation is responsible for the signs and symptoms that affect us all! How do you turn off the heat, redness, swelling and pain when you might not even know it’s there?
Understanding the sugar-inflammation link
Researchers have been exploring the physiological effects of refined sugar on inflammation in the body for some time. It’s been observed that the consumption of refined sugar may trigger various inflammatory mechanisms in the body, including those connected to:
- blood sugar regulation
- immune processes
- metabolic activity
- oxidative stress
By being aware of the potential impacts of refined sugar on inflammation, we can make choices that support our overall health, healing, and goals. This may include finding a balance that works for you individually, considering your own unique dietary needs, preferences, cultural practices, readiness and access to change, and more.
Mechanisms of sugar-induced inflammation
How does excess sugar consumption trigger inflammatory responses?
Blood sugar regulation
As you likely know, consuming sugar causes a rapid spike in blood sugar levels. That spike initiates a release of insulin to regulate the glucose in the bloodstream. Insulin helps deliver the glucose to your cells for energy or storage. But a significant increase in insulin can also have impacts on inflammation, promoting the production of inflammatory molecules.
Immune processes
Refined sugar consumption can also lead to an increase in pro-inflammatory cytokines. These are signaling molecules involved in the inflammatory process. Pro-inflammatory cytokines recruit immune cells to an infected area in the body to help make blood vessels more permeable, allowing immune cells to move more readily into the tissues. This process results in the characteristic signs and symptoms associated with inflammation – redness, swelling, heat, and pain.
Additionally, studies have shown that refined sugar can impair the activity of certain immune cells that play a critical role in defending the body against pathogens. These cells include our front-line immune defenders, the macrophages and neutrophils. This repressed immune cell activity can leave us more vulnerable to the effects of viruses and flus.
Metabolic activity
In addition to the inflammatory process that can be initiated by blood sugar spikes and the subsequent release of insulin, consistent overuse of this physiological response can contribute to challenges with insulin activity in the body. Insulin resistance is one such effect. It can occur when the body’s cells are less responsive to the effects of insulin, continually requiring more insulin to attempt to regulate glucose levels.
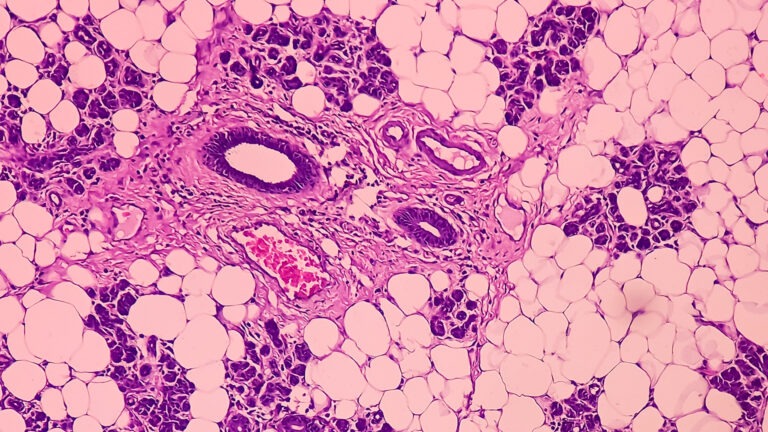
Not only does this raise the potential risks for further internal inflammation, but increased insulin in the bloodstream can contribute to the production of adipose tissue (commonly known as body fat). This tissue can produce additional pro-inflammatory molecules called adipokines. These cells stimulate the production of other inflammatory molecules, contributing to the state of low-grade chronic inflammation.
Oxidative stress
Oxidative stress is a process that occurs when there is an imbalance between the production of reactive oxygen species (ROS) and the body’s ability to neutralize them with antioxidants. Excess refined sugar consumption can contribute to oxidative stress through multiple mechanisms related to how the sugar is metabolized within the body. Dietary sugar goes through a metabolic process called glycolysis, where it’s broken down to produce energy. This process can also generate byproducts such as electrons and oxygen radicals that can contribute to the generation of reactive oxygen species (ROS), leading to oxidative stress.
Functional approaches for addressing sugar-induced inflammation
When we foster an understanding of cause and effect we are not condemning certain foods or those who eat them. This exploration is not about demonizing refined sugar. The impact of sugar consumption will vary among individuals based on a number of factors including genetics, digestion, inflammatory and metabolic health history, nutrient status, and lifestyle factors.
Knowledge is meant to be empowering. Making connections allows us to understand our own daily decisions in relation to risk and reward.
When it comes to mitigating the impacts of refined sugar on existing inflammatory states to turn off that niggling heat, redness, swelling and pain, there are several strategies we like to employ with our clients in the Functional Nutrition Alliance Clinic. Making change to both our habits and our internal terrain takes time. It’s perfectly okay to start slowly and gradually to invite the long term outcomes that you and your clients are after.
Dietary recommendations for reducing sugar consumption and mitigating inflammation
- “Crowd out” refined sugar with lower glycemic (whole food) sweeteners
- Introduce the Fat/Fiber/Protein methodology with every meal or snack
- Eat the rainbow to balance micronutrients and include more antioxidants
By understanding the complex relationship between sugar and inflammation, you have the opportunity to help yourself and others cultivate a healthier and more balanced approach to healing and recovery. Additionally, we want to support others to embrace a mindful and inclusive perspective, where they can develop a positive relationship with food that respects their body’s needs and preferences. Taking steps to address the emotional and psychological aspects of their relationship with sugar can bring about a sense of peace and freedom from cravings. All of this fosters the body’s natural ability to regulate inflammation, reduce the potential risks of disease and promote more resiliency.
EXPERIENCE A FREE TRAINING SERIES WITH ANDREA NAKAYAMA TO HELP YOU
Begin practicing functionally today!
MORE TO EXPLORE
You Might Also Like
Maya Simand: Cancer Survivor to Holistic Cancer Coach
Holistic cancer coach Maya Simand shares her inspiring journey to healing. Discover how Functional Nutrition education empowered her to overcome breast cancer and help others find hope through integrative approaches.
Read MoreEstrogen dominance and breast cancer prevention: A Functional Nutrition approach
Estrogen dominance is a key factor in ER+ breast cancer. This Functional Nutrition guide explores how estrogen dominance increases risk and provides practical strategies to balance hormones and support overall health.
Read MoreThe 3 Roots, Many Branches: A Functional Framework for Clinical Success
As practitioners or aspiring nutrition counselors, we’re all familiar with the frustration of watching people struggle with chronic illness, cycling through symptoms and diagnoses without resolution.
Read MorePutting Patients First with Patient-Centered Care
I recently read an account written by a primary care doctor (PCP) describing a patient who had been passed from one specialist to another—each one focusing on ordering tests, prescribing medications, and ultimately sending her off with more questions than answers. No one paused to truly listen to the patient’s story. No one asked about […]
Read More